85/F with SOB
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 85 F housewife resident of choutuppal came to the OPD with
Chief complaints -
Difficulty in breathing -10 days
HISTORY OF PRESENTING ILLNESS :-
patient was apparently asymptomatic 10 days ago then she complained of shortness of breath which progressed from grade 3- grade 4 according to MMRC.
Aggravated by physical activity.
She has a history of fall 30 days back and sustained injury to right hip for which she was taken to a hospital and was admitted there for 5 days and was diagnosed with right intertrochanteric fracture and received symptomatic treatment and was sent to home for bed rest . After which she developed generalized weakness as the patient's food intake was reduced and later she developed bed sores in the right gluteal region .
No history of fever, cold, burning micturition , chestpain , palpitations, decreased urine output, pedal edema .
Past history :-
She is not a known case of HTN ,DM ,CVA ,CAD ,TB ,ASTHMA.
Personal history:-
Diet :- mixed
Appetite:- decreased
Bowel and bladder:- normal and regular
Sleep:- adequate
Tobacco chewer 1/ day for 30 years
Family history:-
Not significant
General examination:-
Patient is conscious and disoriented
Pallor present
No Icterus
No Cyanosis
No Clubbing
No Lymphadenopathy
No Edema
Vitals :-
Temperature:- afebrile
Pulse rate :- 120
Bp:- 120/70
Respiratory rate :- 24 cpm
Spo2:- 96 at room air
Systemic examination
Respiratory:-
Inspection:-
Chest is bilaterally symmetrical
Trachea – midline in position
Apical Impulse is not appreciated .
No dilated vein ,scars and sinuses
Palpation :-
All inspectory findings are confirmed
Trachea is central in position.
Apex beat not appreciable
Reduced bilateral chest movements are present.
Percussion :-
Dull note was heard over left axillary and infra axillary areas .
Auscultation:-
Bilateral air entry - present
Vesicular breath sounds heard
Bilaterally decreased breath sounds.
Cardiovascular system:-
•Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
•S1 and S2 heard , no added thrills and murmurs heard.
Per abdomen:-
INSPECTION
Shape of abdomen appears to be Normal
No Visible epigatric veins
No engorged veins sinus scars
PALPATION
All inspectory findings conformed
Abdomen soft & Non tender
No organomegaly
PERCUSSION
Tympanic note heard all quadrants abdomen
AUSCULTATION
Bowel sounds heard.
CNS examination :-
No focal neruological deficit.
Investigations:-
On 16/08/23
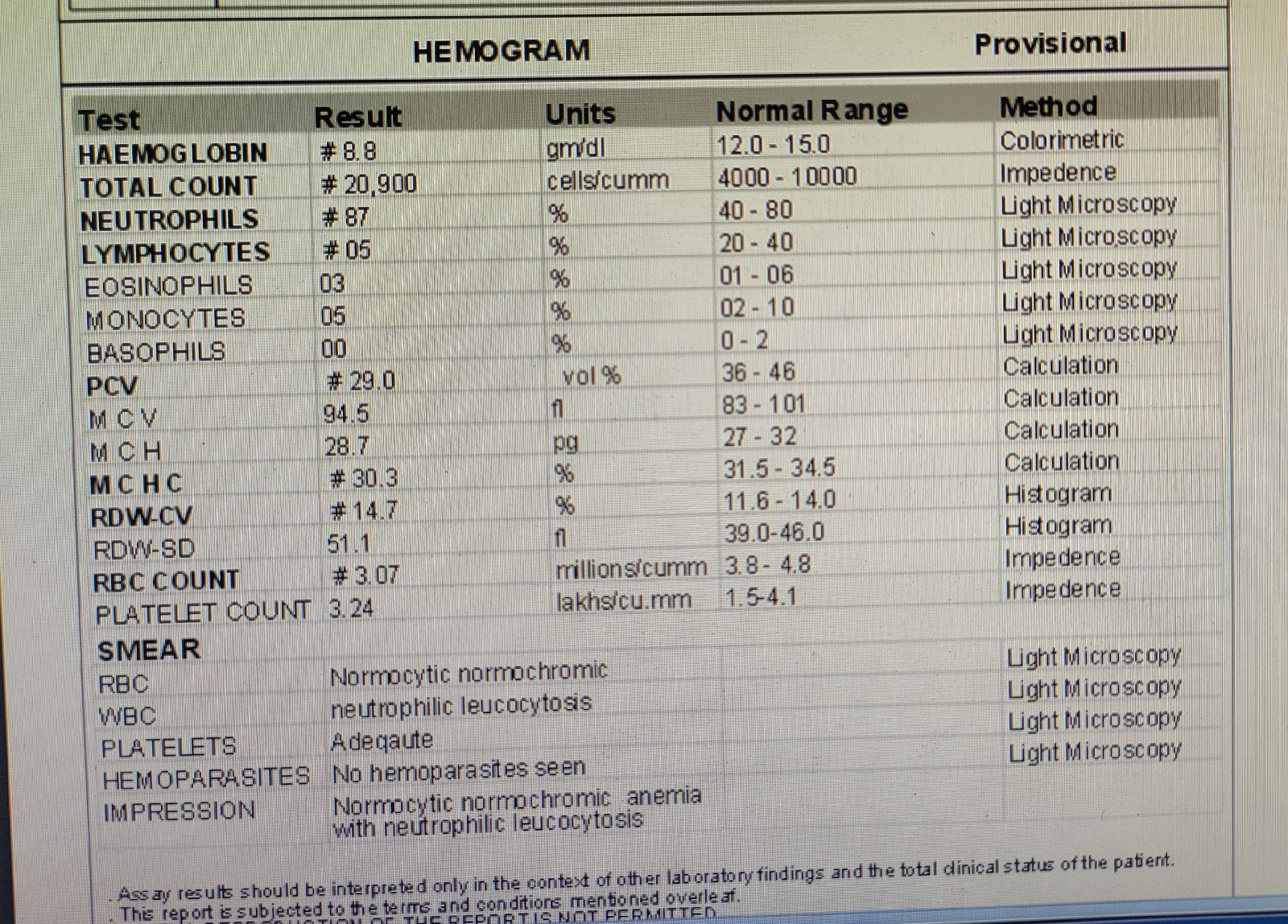
Hemogram :
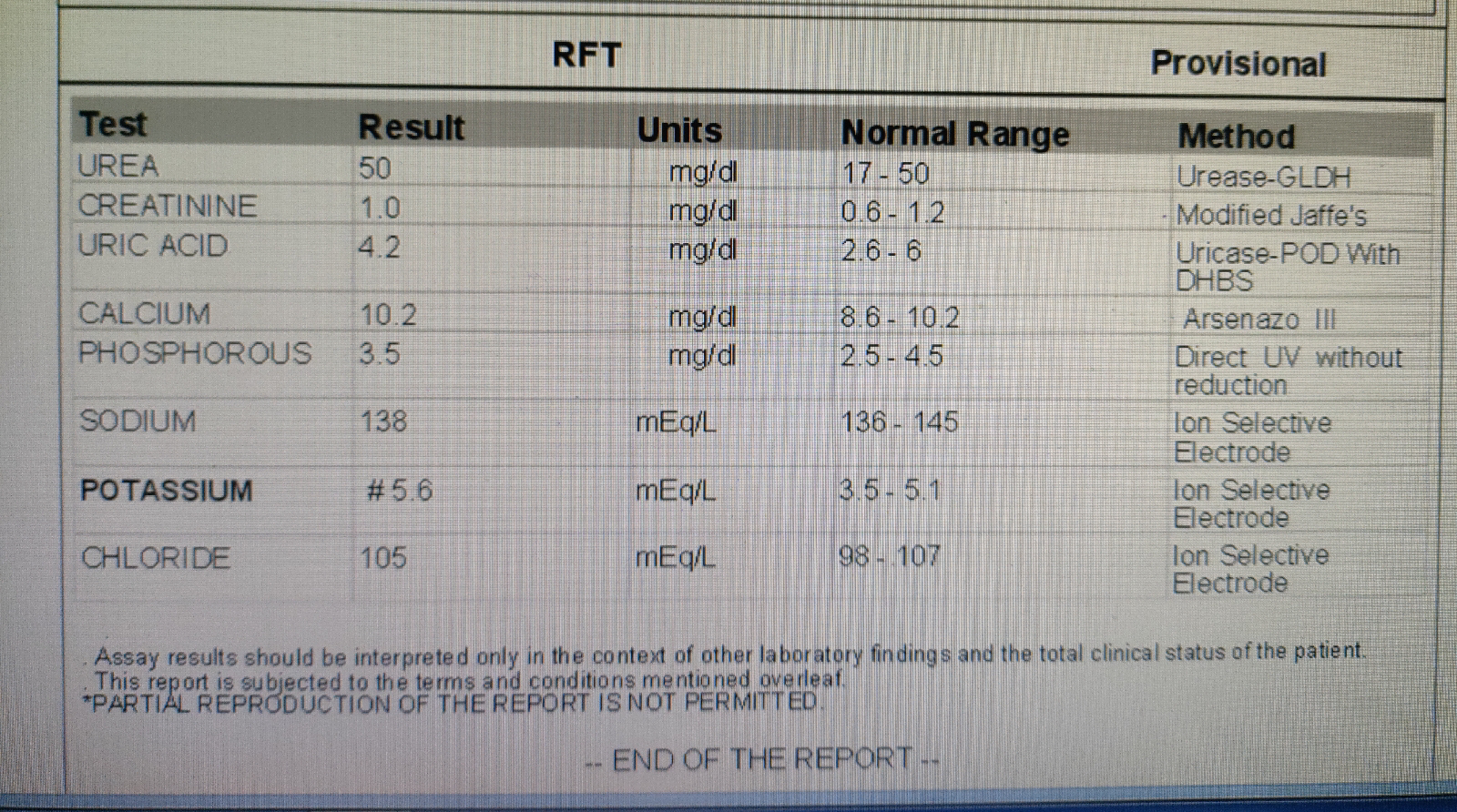
RFT:-
On 17/08/23
D-dimer
CUE
Serum electrolytes
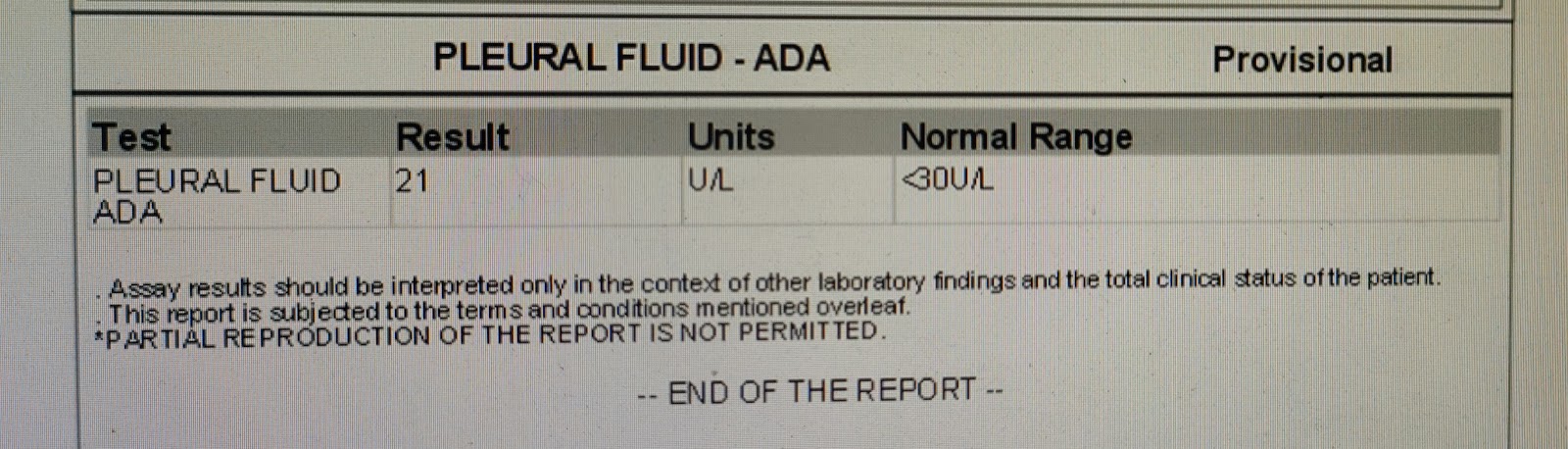
Pleural (sugar,protein)
On 20/08/23
Provisional diagnosis:-
?Pulmonary emobolism
?Emphysema.















Comments
Post a Comment